Florida Medicaid Provider Enrollment
A provider must visit the website and complete the application by choosing the Provider Service Tab’s enrolment option in order to become a part of the Florida Medicaid program. The purpose of the Florida Medicaid Provider Enrollment Application is to collect data on a candidate’s eligibility for Florida Medicaid.
How to Check Enrollment Status
- Providers are strongly encouraged to use the Enrolment Tracking Search to view and verify the current status of their application(s).
- Enter your ATN, then your last name or business name, to find out the status of your application.
- The name, including any unusual characters, must be entered precisely as it appears on the application. After entering the correct data, select “Search.”
- A Search Results panel will follow the Enrollment Tracking Search window.
- The Status column’s first row shows the application’s status, while the following rows show the status of every application module.
- Additionally, providers have the option to upload files from this panel or print a copy of the application.
Florida Medicaid Provider Enrollment Background Screening
To enroll as a Florida Medicaid, healthcare providers must submit a Florida Medicaid provider enrollment background screening. Before any employee is employed for a position that calls for this kind of screening, the Background Screening Unit analyses these checks to make sure they all fulfill the eligibility requirements.
Florida Medicaid Provider Enrollment Status Guide
| Application Status Codes | Explanation | Timeline |
| Not Submitted | The application has not yet been submitted to Medicaid for processing. Before processing can start, the applicant must log in, finish all sections of the application, and submit. | Awaiting Provider |
| Awaiting Supporting Documents | The application has been submitted; however, before processing can start, the applicant must upload the necessary supporting documentation, which is indicated in the search results above. | Awaiting Provider |
| In process | The application is being reviewed to check accuracy and eligibility of the provider | Almost 14 business days |
| Background Screening | Waiting for the results from background screening departments | Almost 5 business days |
| QC | Application is being checked for accurate handling | Almost 5 business days |
| Application Deficient | The application or supporting documentation was incomplete. The applicant received a letter outlining the items that needed to be corrected and resubmitted. Deficiencies lengthen the time it takes to process the enrolment application. The most frequent application deficiencies are: Background screening results have not been received or indicate an ineligible statusMissing the required supporting documentationApplicants are sending individual documents rather than all required documentation at onceSupporting documents are not verified and signed by an unauthorised signer.Mismatched or Wrong proof of Tax ID | Awaiting Provider |
| Clearing House | Waiting for background screening results | < 15 calendar days |
| State Review | Applications with the status “State Review” will indicate that they are awaiting Agency verification. The State Review involves verifying the data on an enrolment application, including certificate and dates of expiration, looking up the applicant’s past interactions with Medicaid or other state departments, and examining the applicant’s economic background. | |
| Ownership Transition for Facility Providers | How long a review takes facility providers depends on whether a survey or rate setting is necessary before rates are made public. | |
| Transfer of Ownership for Non-Facility Providers | Less than 15 Days | |
| Establishing Facility Rates | Depending on the type of facility | |
| In-person meeting | < 60-Day | |
| Pre-Certification Survey for Residential or Behavioural Medical Services | < A Year | |
| Prior Refusal, Termination, or Context Examining | About three working days | |
| Enrolled | Provider authorised. After the new provider is activated, a welcome letter will be mailed two business days later. A Florida Medicaid Secure Web Portal PIN Letter will also be mailed to applicants. To access their protected Web Portal account, providers must adhere to the PIN Letter instructions carefully. | Approximately five business days after all enrolment conditions, including receiving an eligibility screening, are met, approved applications become active. Findings from the Clearinghouse for Background Screening. |
| Refused | The application has been closed and is incomplete because of inactive behavior or other reasons. If the candidate decides to pursue enrolling, a fresh application has to be sent in. | N/A |
| Closed | The application has been closed and is incomplete because of inactivation of provider. If the candidate decides to pursue enrolling, a fresh application has to be sent in. | N/A |
Providers are urged to use the Web Chat tool when they have questions or concerns about their application. Click the green button at the bottom-right corner of the search results box to start a web chat.
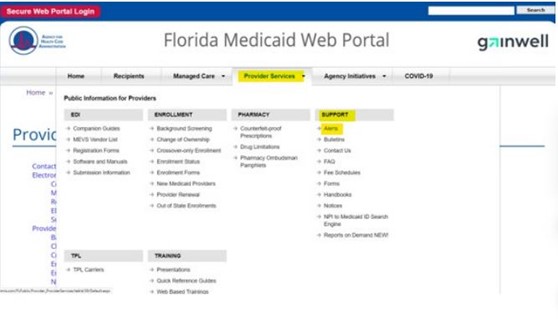
Florida Medicaid Provider Enrollment Status Portal
You can go to the official Florida Medicaid portal and use your login information to access your provider enrolment account. If you recently altered your password, ensure that you use a fresh one.
- You should go to Florida Web Portal
- Click login option
- Add your user name/ email address
- Put the correct password
- You can have options to change your password via mail link if you forget your password
Making Modifications to an Incomplete Application
If the application or supporting material is incomplete or lacks relevant information, applicants will need to use the Correct Application or Upload Material options on the Enrollment Tracking Search page. If an applicant decides they no longer want to pursue enrollment, they can use the Cancel Application option to discontinue their current application.
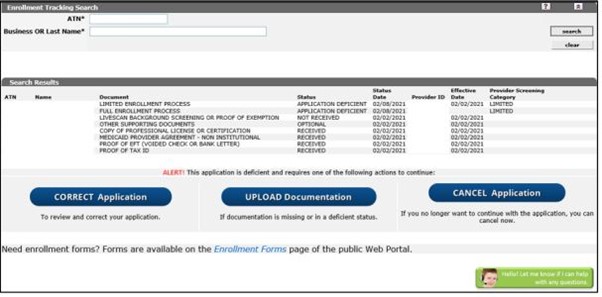
Appropriate Use
Using the Online Enrollment Wizard, applicants can instantly edit and fix their applications that are listed as application-deficient. Additional location codes or providers from outside the state are not eligible for this capability.
The applicant will be able to complete the application in its entirety if the Correct Application option is chosen.
Applicants cannot alter the following:
- Application type
- CHOW indicator (Yes/No)
- Enrollment type; Provider type
- Tax ID type and Tax ID (Identifying Information panel)
- Electronic Funds Transfer (EFT)
Attach Documents
Candidates may employ the Upload Documentation feature to upload the appropriate documents if any are missing or in a deficient state.
It does not handle modifications made from printed applications using the option of Upload Documentation option. Providers need to select the Correct Application option to change their pending application.
Cancel Application
The candidate can choose to cancel or terminate their pending application by going to the Enrollment Application Status tab and selecting the Cancel Application options. If the applicant wants to reapply in the future, they will need to establish a new application because this decision is final.
Florida Medicaid Provider Enrollment Status Phone Number
1-877-711-3662 is the contact number for the questions regarding enrolment as Medicaid providers in Florida. Their team are available at reception and they are open from 8 a.m. to 8 p.m.